Psoriasis treatment aims to control inflammation, reduce scaling, and improve quality of life using a stepwise approach tailored to disease severity, location, and patient preferences.
What is psoriasis?
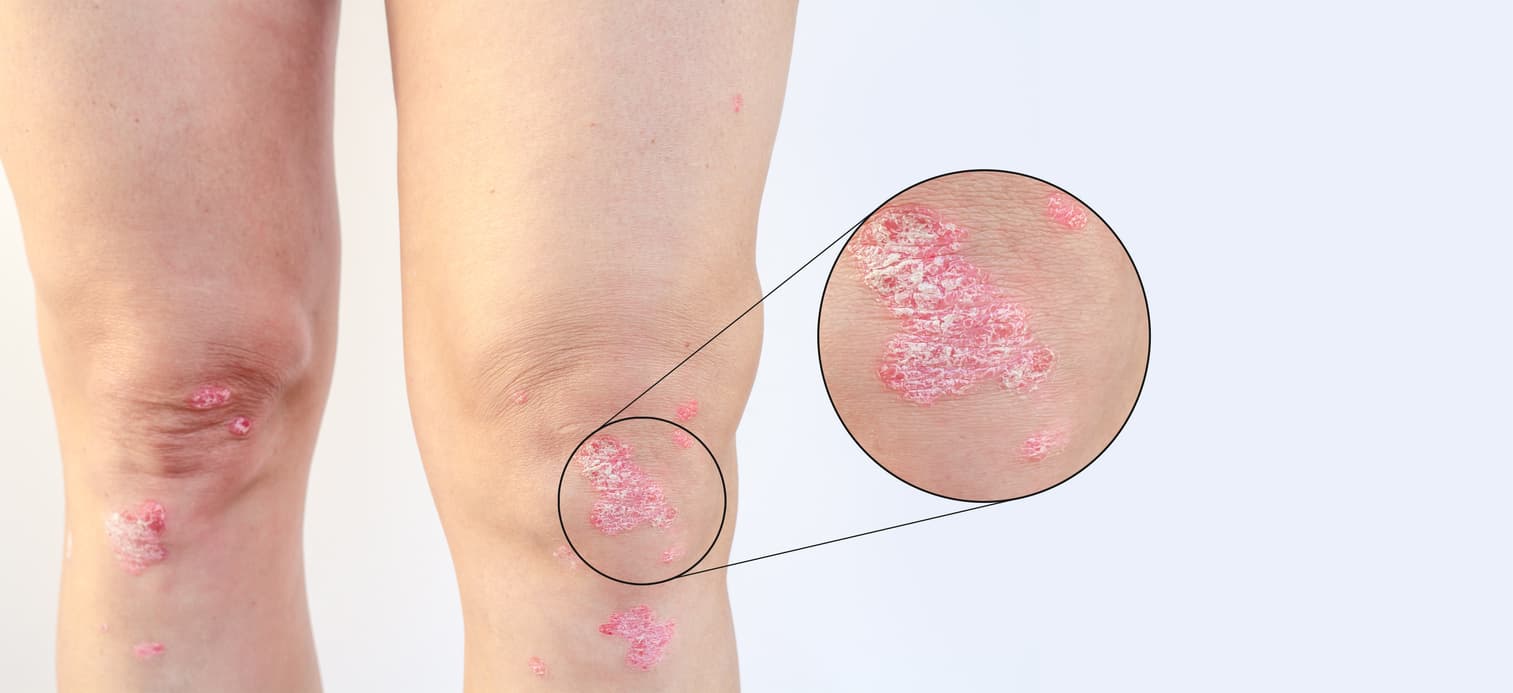
Psoriasis is a chronic, immune‑mediated inflammatory skin disorder characterized by accelerated skin cell turnover that produces well‑demarcated, red plaques covered by silvery scale. The condition arises from dysregulated interactions between the innate and adaptive immune systems and keratinocytes, leading to persistent inflammation, epidermal hyperproliferation, and altered barrier function. Clinical presentations vary widely: plaque psoriasis is the most common form, but guttate, inverse, pustular, and erythrodermic types occur and can differ in distribution, severity, and triggers. Lesions commonly appear on extensor surfaces, the scalp, nails, and the lumbosacral area, and they may be itchy, painful, or bleed with trauma. Psoriasis follows a relapsing–remitting course influenced by genetic predisposition and environmental factors such as infections, skin injury, stress, certain medications, and metabolic or lifestyle factors. Beyond the skin, psoriasis is associated with systemic inflammation and an increased risk of comorbidities including psoriatic arthritis, cardiovascular disease, metabolic syndrome, and mood disorders, making holistic assessment important. Diagnosis is usually clinical and sometimes supported by biopsy, while management focuses on reducing inflammation, controlling symptoms, preventing complications, and improving quality of life through topical treatments, phototherapy, and systemic or biologic agents chosen according to disease severity and patient needs.

What part of my body will psoriasis affect?
Psoriasis can appear almost anywhere on the body, but certain sites are particularly common and have distinct clinical patterns and management implications.
The most frequent locations are the elbows and knees, where well defined scaly plaques develop on extensor surfaces.
The scalp is another typical site; scalp psoriasis ranges from small, flaky patches along the hairline to extensive involvement beneath hair that can be itchy and difficult to treat.
The nails are often affected, producing pitting, discoloration, thickening, and separation of the nail plate from the nail bed.
Psoriasis also commonly occurs on the lower back and buttocks, and in skin folds such as the groin, armpits, and under the breasts, where the lesions are smoother and less scaly.
Less common but more severe presentations include widespread body involvement called erythrodermic psoriasis and pustular psoriasis that forms pus-filled bumps on the palms, soles, or generalized areas.
About 30 percent of people with psoriasis develop joint inflammation known as psoriatic arthritis, which typically affects the fingers, toes, spine, or large joints.
Distribution varies with age, psoriasis subtype, genetics, and triggers, and involvement of visible or sensitive areas often has a disproportionate impact on quality of life.
What are the symptoms & causes of psoriasis?
Psoriasis is a chronic immune‑mediated skin disease marked by accelerated skin cell turnover that produces well‑defined, red or discolored plaques topped with silvery scale, often accompanied by itching, burning, tenderness, or bleeding when lesions are traumatized; nail changes such as pitting, thickening, or onycholysis are common, and some people develop joint pain and stiffness consistent with psoriatic arthritis. Symptoms vary by subtype—plaque psoriasis causes raised scaly patches, guttate presents as numerous small droplets, inverse affects skin folds with smooth red lesions, pustular forms produce pus‑filled bumps, and erythrodermic psoriasis can cause widespread redness and systemic symptoms. The condition arises from a complex interplay of genetic susceptibility and environmental triggers: immune dysregulation—particularly T‑cell and cytokine‑driven inflammation—drives keratinocyte hyperproliferation, while infections, skin injury (Koebner phenomenon), certain medications, stress, smoking, alcohol, and metabolic factors commonly precipitate or exacerbate flares. Psoriasis follows a relapsing‑remitting course influenced by these triggers and underlying comorbidities; diagnosis is usually clinical and management targets reducing inflammation, controlling symptoms, and addressing associated systemic risks.

How is psoriasis managed?
Psoriasis management uses a stepped, individualized approach that combines topical therapies, phototherapy, systemic medications, and lifestyle measures to control inflammation, reduce scaling, and improve quality of life.
For limited or mild disease, topical corticosteroids, vitamin D analogues, calcineurin inhibitors, keratolytics, and emollients are first-line to relieve symptoms and restore barrier function.
When plaques are more extensive or refractory, phototherapy (narrowband UVB or PUVA) offers an effective non‑systemic option that slows keratinocyte proliferation and modulates immune activity.
Moderate to severe disease, or psoriatic arthritis, often requires systemic treatment: conventional oral agents (methotrexate, cyclosporine, acitretin), targeted small molecules (apremilast), or biologic therapies that inhibit specific cytokines and immune pathways, chosen based on efficacy, comorbidity profile, monitoring needs, and patient preference.
Adjunctive measures include smoking cessation, weight management, stress reduction, treatment of infections, and optimizing skin care with gentle cleansers and regular moisturization. Regular follow-up enables treatment escalation, safety monitoring, and assessment for comorbidities such as cardiovascular risk and metabolic syndrome.

What are psoriasis invasive treatment options?
Invasive treatment options for psoriasis are reserved for moderate to severe disease or cases unresponsive to topical therapy and include systemic medications, biologic injections or infusions, and select procedural therapies that require specialist oversight.
Systemic conventional agents such as methotrexate, cyclosporine, and acitretin act broadly to suppress immune-driven keratinocyte proliferation and are administered orally or by injection with regular laboratory monitoring for hepatotoxicity, nephrotoxicity, and other adverse effects.
Biologic therapies—monoclonal antibodies or receptor fusion proteins delivered subcutaneously or intravenously—target specific immune mediators (TNF, IL‑12/23, IL‑17, IL‑23) and provide highly effective, often durable clearance for many patients but require screening for infections and periodic safety surveillance. Small‑molecule oral agents like apremilast offer targeted intracellular modulation with a different safety profile.
Photopheresis and hospital‑based phototherapy protocols are more specialized options for refractory or erythrodermic disease and involve extracorporeal blood treatment or supervised UVA exposure after photosensitizer administration.
In rare scenarios, surgical approaches to manage localized complications—nail surgery or excision of problematic plaques—may be considered.
Choice among these invasive options balances’ disease severity, comorbidities, pregnancy plans, monitoring capacity, infection risk, and patient preferences and should be made in partnership with a dermatologist or rheumatologist.

Can psoriasis be permanently cured?
There is currently no known permanent cure for psoriasis; it is a chronic, immune‑mediated condition that tends to follow a relapsing–remitting course, but modern treatments can suppress disease activity to the point of long periods of remission and, for many people, near‑complete clearance of skin lesions. For now, realistic goals are durable remission, symptom relief, improved quality of life, and regular monitoring for comorbidities under the guidance of a dermatologist.

Conclusion
Effective psoriasis management requires a personalized, multifaceted approach that balances disease severity, comorbidities, patient preferences, and safety considerations; topical therapies and emollients remain foundational for mild disease, phototherapy offers a noninvasive option for more extensive involvement, and systemic agents—including targeted biologics and small molecules—deliver powerful disease control for moderate to severe or refractory cases. Long‑term success depends on shared decision making with a dermatologist, regular monitoring for treatment efficacy and adverse effects, and attention to lifestyle factors that influence flares and overall health. While psoriasis is chronic and not yet curable, modern therapies can achieve sustained remission, markedly improve quality of life, and reduce the risk of systemic complications when treatments are chosen thoughtfully and combined with ongoing preventive care.
Read More
