Hydrotherapy and aquatic therapy both use water to support healing and exercise, but hydrotherapy emphasizes water’s physical properties (temperature, pressure, buoyancy) for passive and active treatments, while aquatic therapy is a structured, therapist‑led exercise program performed in a pool to restore function and mobility.
What is hydrotherapy?
Hydrotherapy, also called water therapy or balneotherapy, is any therapeutic use of water to treat symptoms and support recovery across a wide range of conditions. It encompasses passive modalities such as warm or cold baths, contrast baths, and whirlpool immersion, as well as active approaches like therapeutic exercise in a warm pool where buoyancy reduces joint load and hydrostatic pressure assists circulation. Practitioners exploit water’s temperature to modulate pain and muscle tone, buoyancy to decrease weight‑bearing and enable earlier movement after injury or surgery, hydrostatic pressure to reduce edema and support venous return, and mechanical forces (jets, currents) to provide massage‑like effects and stimulate circulation. Hydrotherapy is used in musculoskeletal rehabilitation (arthritis, post‑operative recovery), neurological conditions (stroke, multiple sclerosis), chronic pain syndromes (fibromyalgia), and for wound care and edema management; it can be delivered in clinical settings by licensed therapists or as adjunctive spa treatments for symptom relief. Key benefits include pain reduction, improved range of motion, enhanced functional mobility, and the ability to perform progressive strengthening with lower joint stress.

What is aquatic therapy?
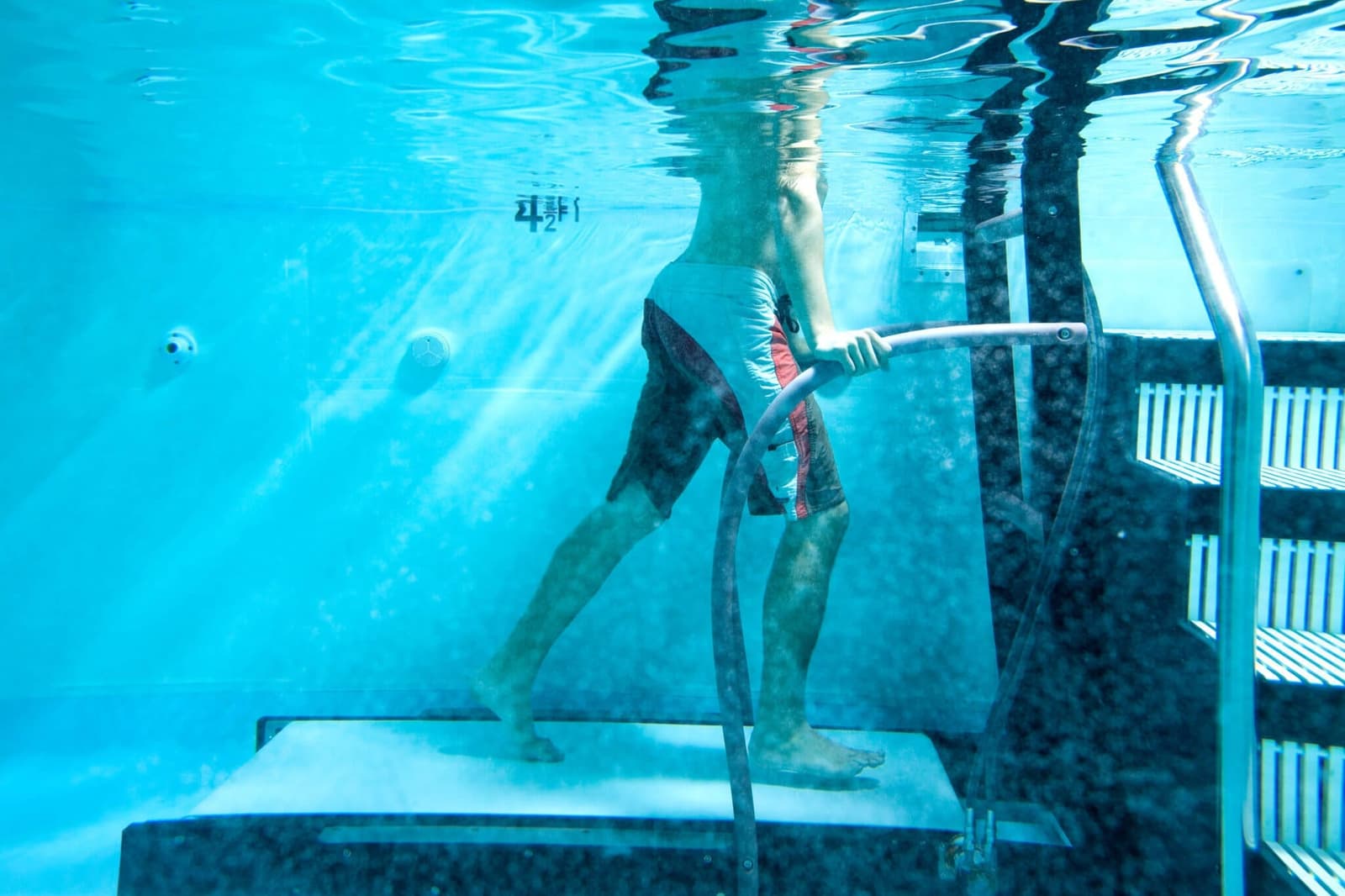
Aquatic therapy, also called aquatic rehabilitation or aquatherapy, is a specialized form of physical and occupational therapy that uses a pool environment to deliver therapeutic exercise, manual techniques, and functional training. Sessions are typically led by a licensed therapist who tailors movements to the patient’s goals, exploiting water’s unique properties—buoyancy to reduce weight‑bearing, hydrostatic pressure to assist circulation and reduce swelling, thermal effects to relax muscles, and water resistance to provide graded strengthening. Common techniques include gait training, balance and coordination drills, progressive strengthening, and specialized methods such as Halliwick, Bad Ragaz, and Ai Chi that combine motor control and breathing work. Aquatic therapy is used across the lifespan for postoperative orthopedic recovery, chronic pain, arthritis, neurological conditions (stroke, spinal cord injury, multiple sclerosis), pediatric disabilities, and fall‑prevention programs; the warm, supportive environment often enables earlier and safer movement than land‑based therapy. Sessions may be individual or group based, and therapists monitor intensity, water temperature, and progression to meet functional goals while minimizing joint stress and pain.

Why is hydrotherapy used?
Hydrotherapy harnesses water’s thermal effects to modulate pain and muscle tone: warm immersion relaxes muscles, increases local blood flow, and can reduce stiffness, while cold applications help control inflammation and acute pain. Clinicians use contrast baths, warm whirlpools, and localized soaks to exploit these temperature responses for symptom control and comfort during recovery.
Water’s buoyancy is another central reason hydrotherapy is prescribed: by offloading body weight, buoyancy reduces joint compression and pain, allowing patients to begin movement and strengthening earlier than on land. This makes hydrotherapy especially valuable after orthopedic surgery, for arthritis, and for people who cannot tolerate full weight bearing during early rehabilitation.
Hydrostatic pressure and mechanical forces in water also provide therapeutic advantages. Hydrostatic pressure helps reduce peripheral edema and supports venous return, while jets and currents create graded resistance and massage‑like stimulation that improve circulation and soft‑tissue mobility. Therapists use these properties to progress balance, gait, and functional tasks in a low‑fall‑risk environment, and to deliver cardiovascular conditioning with lower joint stress than land‑based exercise.
Why is aquatic therapy used?
Aquatic therapy is prescribed to restore function, reduce pain, and accelerate recovery by taking advantage of water’s physical characteristics. Buoyancy reduces effective body weight, allowing patients to move with less joint compression and pain, which makes early mobilization and gait training possible after surgery or injury.
Hydrostatic pressure helps control swelling and supports venous return, improving comfort and circulation during exercise. Warm water promotes muscle relaxation and decreased spasm, while water resistance provides a graded, multidirectional load for strengthening and endurance without the high impact of land‑based exercise.
Therapists use these features to design individualized programs—gait retraining, balance and coordination drills, progressive strengthening, and cardiovascular conditioning—that are safer for people with arthritis, postoperative limitations, neurological impairments, or deconditioning. Aquatic methods such as Halliwick, Bad Ragaz, and Ai Chi combine motor control, breathing, and functional tasks to transfer gains back to land‑based activities.
The pool environment also lowers fall risk and often improves patient confidence and adherence, which can speed functional gains and reduce pain‑related fear of movement. Clinical centers and rehabilitation programs increasingly integrate aquatic therapy as a complement to land therapy because it enables earlier, more comfortable exercise progression and supports complex functional goals.

hydrotherapy vs. aquatic therapy; which is best for me?
Hydrotherapy broadly refers to therapeutic uses of water—warm or cold immersion, whirlpools, contrast baths, and targeted jets—to modulate pain, circulation, muscle tone, and wound or edema care. It often focuses on symptom control and passive modalities that exploit temperature and mechanical forces for short‑term relief. Aquatic therapy (aquatic rehabilitation) is a structured, clinician‑designed exercise program performed in a pool where buoyancy reduces weight bearing, hydrostatic pressure helps edema, and water resistance provides graded strengthening; it emphasizes functional recovery, gait training, balance, and progressive strengthening under professional supervision.
If your primary goal is short‑term pain relief, muscle relaxation, or wound/edema care, hydrotherapy may be the simpler, effective option. If you need postoperative rehabilitation, improved gait, balance, strength, or neurological recovery, aquatic therapy is usually better because it is therapist‑led and progressive. Choose aquatic therapy when you require measurable functional gains; choose hydrotherapy for symptom control or adjunctive comfort. For mixed needs, many programs combine both approaches to maximize comfort and function.

Conclusion
Hydrotherapy focuses on water’s physical effects for symptom relief, while aquatic therapy is a therapist‑led exercise program in a pool to restore function; choose hydrotherapy for passive pain control and aquatic therapy when you need structured rehabilitation.
Read More
