Symptoms of Pancreas Problems vary widely—abdominal pain, nausea, weight loss, steatorrhea, or abnormal glucose control—and severity ranges from transient, self‑limited illness to life‑threatening disease that requires urgent care or surgery.
What are the symptoms of having Pancreas Problems?
Abnormalities of the pancreas often produce a recognizable constellation of symptoms that reflect inflammation, obstruction, or loss of function.
The most common complaint is abdominal pain, typically located in the upper abdomen and sometimes radiating to the back, which can be severe and constant or intermittent.
Nausea and vomiting frequently accompany acute inflammation or bowel irritation, and patients may develop fever if infection or systemic inflammation is present.
When exocrine function is impaired, stools become oily, pale, bulky, and foul-smelling because fats are poorly absorbed, and chronic malabsorption leads to unintentional weight loss despite normal appetite.
Jaundice — yellowing of the skin and eyes — signals biliary obstruction from a mass in the pancreatic head or pancreaticobiliary inflammation and warrants prompt evaluation.
On physical exam the abdomen may be tender to palpation, sometimes with guarding, and signs of systemic illness such as rapid pulse or low blood pressure indicate more severe disease.
Together, these features — abdominal pain, nausea and vomiting, fever, oily malodorous stools, jaundice, abdominal tenderness, and unintended weight loss — should prompt timely medical assessment since early diagnosis and targeted treatment improve outcomes and reduce the risk of complications.
What is pancreatitis?
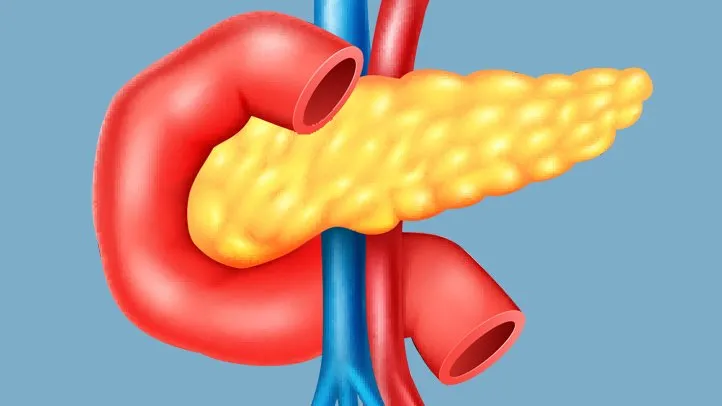
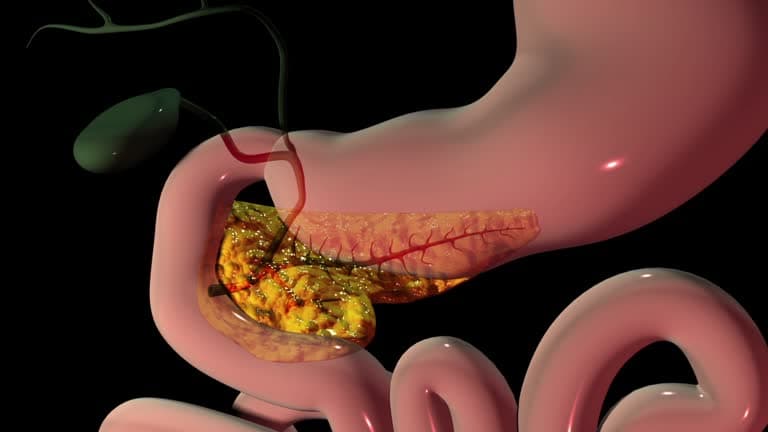
Pancreatitis is inflammation of the pancreas, a flat gland behind the stomach that produces digestive enzymes and hormones such as insulin; when these enzymes activate prematurely inside the gland they cause self‑digestion, swelling, pain, and impaired pancreatic function. Pancreatitis may present as an acute, sudden illness that ranges from mild, self‑limited inflammation to severe, life‑threatening systemic disease with organ failure and local complications such as necrosis, abscess, or fluid collections. It can also be chronic, with persistent inflammation that leads to progressive fibrosis, loss of exocrine and endocrine function, recurrent abdominal pain, malabsorption, and diabetes. Common causes include gallstones that obstruct the pancreatic duct and heavy alcohol use, but other triggers are hypertriglyceridemia, medications, autoimmune conditions, trauma, structural ductal abnormalities, and infections. Diagnosis relies on a combination of characteristic abdominal pain, elevated pancreatic enzymes in the blood, and imaging findings. Management depends on severity and cause: initial treatment for acute pancreatitis emphasizes fluid resuscitation, pain control, and organ support, while chronic pancreatitis focuses on pain management, nutritional support, enzyme replacement, and treating complications; addressing the underlying cause helps prevent recurrence.

What are the different types of pancreatitis?
Acute pancreatitis is a sudden inflammation of the pancreas that typically presents with severe, often constant upper abdominal pain that can radiate to the back, accompanied by nausea, vomiting, and elevated pancreatic enzymes; it ranges from a mild, self‑limited illness managed with fluid resuscitation, pain control, and short hospital observation to a fulminant systemic disease with necrosis, infected collections, multi‑organ failure, and prolonged critical care needs. Common precipitants include gallstones obstructing the pancreatic duct, heavy alcohol use, hypertriglyceridemia, certain medications, trauma, and endoscopic procedures, and diagnosis rests on characteristic symptoms, blood tests, and imaging.
Chronic pancreatitis is a progressive, long‑standing inflammatory condition in which repeated injury produces fibrosis, permanent loss of exocrine and endocrine function, recurrent or chronic abdominal pain, malabsorption with fatty, foul‑smelling stools, and diabetes; causes overlap with acute disease but emphasize prolonged alcohol exposure, genetic predisposition, autoimmune disease, and ductal abnormalities. While acute episodes may resolve completely, recurrent acute attacks can evolve into chronic disease.
Management differs, acute care focuses on stabilization and treating the trigger (for example, gallstone removal), whereas chronic disease management emphasizes pain control, pancreatic enzyme replacement, nutritional support, management of diabetes, endoscopic or surgical interventions for complications, and multidisciplinary long‑term follow‑up.
When to see a doctor for your pancreas?
Seek medical attention promptly if you experience sudden, severe upper abdominal pain—especially if it radiates to your back—or if pain is accompanied by persistent nausea, vomiting, fever, rapid pulse, fainting, or difficulty breathing, because these can signal acute pancreatitis or a complication that requires urgent care. See a clinician soon for new or worsening chronic upper abdominal discomfort, unintentional weight loss, persistent oily or foul-smelling stools, or new-onset diabetes, as these symptoms may indicate chronic pancreatitis, exocrine insufficiency, or an obstructing lesion. Jaundice (yellowing of the skin or eyes), dark urine, or pale stools warrant rapid evaluation because they suggest bile duct obstruction, which can be caused by tumors in or near the pancreas. If you have risk factors such as heavy alcohol use, gallstones, very high triglycerides, a family history of pancreatic disease, or genetic conditions associated with pancreatitis, discuss screening and preventive measures with your doctor even when symptoms are mild. For any unexplained, persistent digestive symptoms or systemic signs of illness, early assessment allows timely diagnosis with blood tests and imaging, prompt treatment to reduce complications, and a coordinated plan for follow‑up care with gastroenterology, surgery, nutrition, and endocrinology as needed.
How is pancreatitis treated?
Treatment for pancreatitis depends on whether it is acute or chronic and on severity, but the overarching goals are to relieve pain, support organ function, treat the underlying cause, and prevent or manage complications.
Initial care for acute attacks often requires hospital admission for aggressive intravenous fluids, pain control with analgesics, and careful monitoring of vital signs and laboratory values; patients are usually kept NPO (no oral intake) until nausea, vomiting, and pain improve, with gradual reintroduction of oral or enteral nutrition as tolerated.
If infection, necrosis, or persistent ductal obstruction is present, antibiotics, endoscopic procedures (such as ERCP to remove gallstones or place stents), percutaneous drainage of fluid collections, or surgery to debride necrotic tissue may be needed.
Chronic pancreatitis treatment focuses on long‑term pain management, pancreatic enzyme replacement to treat malabsorption, nutritional support and vitamin supplementation, alcohol cessation and management of metabolic triggers like hypertriglyceridemia, and diabetes care when endocrine function is impaired.
Endoscopic or surgical interventions relieve ductal obstruction or complications for refractory pain or complications, and a multidisciplinary approach involving gastroenterology, surgery, nutrition, and endocrinology optimizes outcomes and reduces recurrence.
How to prevent pancreatitis?
Preventing pancreatitis focuses on addressing common triggers and adopting sustained healthy habits that reduce the risk of both acute attacks and progression to chronic disease.
Key measures include avoiding heavy alcohol use and quitting smoking, since both are major, modifiable risk factors; moderating alcohol and eliminating tobacco substantially lower recurrence risk. Managing gallstone disease—through timely evaluation and, when indicated, cholecystectomy—prevents stone‑related duct obstruction that commonly precipitates acute pancreatitis.
Control metabolic contributors such as hypertriglyceridemia with diet, medication, and weight management to reduce pancreatitis caused by very high triglyceride levels. Adopt a pancreas‑friendly diet rich in lean proteins, whole grains, low‑fat dairy, fruits and vegetables while limiting fried, fatty, and highly processed foods; portion control and gradual weight loss for those with obesity are protective.
Stay hydrated and seek early medical review for biliary colic, persistent upper abdominal pain, or unexplained digestive changes.
For people with recurrent or idiopathic pancreatitis, pursue specialist evaluation for genetic, autoimmune, or anatomic causes that may be treatable; follow-up care with gastroenterology, nutrition, and primary care supports risk‑reduction strategies.
These combined lifestyle, medical, and procedural steps lower the chance of initial and recurrent pancreatitis episodes.

Conclusion
Pancreatic problems often present with a cluster of symptoms that together point to underlying inflammation, obstruction, or functional loss: the hallmark is persistent upper abdominal pain that may radiate to the back, frequently accompanied by nausea and vomiting, fever with systemic illness, and abdominal tenderness. Functional impairment produces oily, foul‑smelling stools and unintended weight loss from malabsorption, while biliary obstruction or a mass can cause jaundice with yellowing of the skin and dark urine. Because these signs range from mild and intermittent to sudden and life‑threatening, recognizing symptom patterns—severe acute pain, progressive weight loss, new steatorrhea, or new‑onset diabetes—matters; early medical assessment enables timely diagnosis with blood tests and imaging, rapid treatment of acute complications, and initiation of long‑term care to preserve nutrition and metabolic health.
Read More
