Sperm donation is the voluntary provision of sperm to help others achieve pregnancy through assisted reproductive techniques; it is regulated by sperm banks and fertility clinics and involves medical screening, sample collection, testing, and storage or immediate use.
What is sperm donation?
Sperm donation is the provision of sperm by a man with the intention that it be used in artificial insemination or other fertility treatments for people who are not his sexual partners. Donors produce semen samples at a clinic or sperm bank; samples are evaluated for count, motility, and morphology, then undergo infectious‑disease testing, genetic screening, and quarantine before being accepted for use or cryopreservation. Accepted samples are frozen and stored under strict conditions and can be supplied to recipients for intrauterine insemination (IUI) or in vitro fertilization (IVF), or used with a gestational carrier when needed. Programs vary in whether donors remain anonymous or agree to future contact, and recipient families select donors based on medical history and available profiles; legal arrangements typically clarify that donors relinquish parental rights when donation is performed through regulated channels.
What happens before sperm donation?
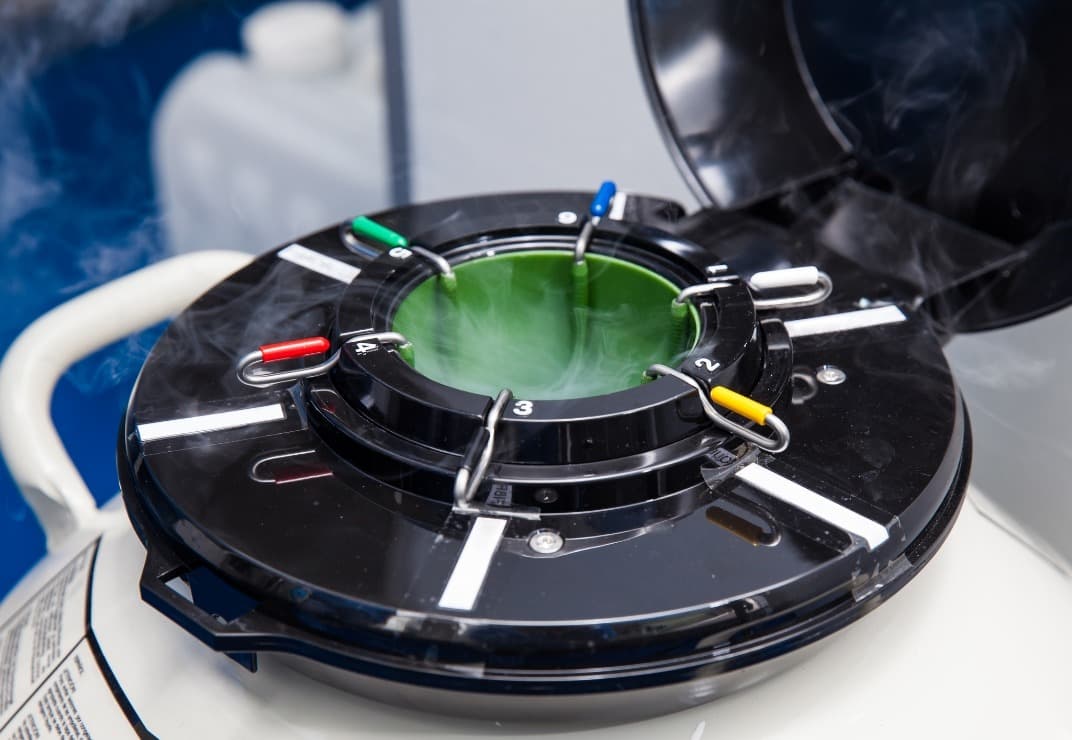
Most sperm donation journeys begin with an initial inquiry and application where basic eligibility—age, general health, and lifestyle—is assessed. If pre‑screening looks promising, you’ll complete a detailed medical and family history questionnaire and provide consent for genetic carrier screening and infectious‑disease testing. Clinics require a semen analysis to measure count, motility, and morphology, and you’ll be asked to abstain from ejaculation for about 48–72 hours before providing a sample to optimize quality. Donors typically produce samples at the clinic under controlled conditions; accepted samples are frozen (cryopreserved) and placed in quarantine while repeat infectious testing and confirmatory analyses are completed. Many programs request multiple visits and samples to ensure consistent quality and to build a usable inventory. Psychological screening or counseling and clear legal agreements about parental rights and anonymity are standard parts of the pre‑donation process. Donor profiles and matching options are discussed with recipients, and reputable banks explain storage, matching, and record‑keeping policies before you commit.

Who benefits from donated sperm?
Donated sperm benefits a wide range of people who want to become parents but cannot rely on sperm from an intended father: couples facing male factor infertility (including low sperm count, poor motility, or azoospermia), single women choosing parenthood, lesbian couples and some transgender individuals, and people or couples seeking to avoid passing on serious genetic conditions; it also helps patients whose fertility was impaired by cancer treatments and others for whom biological paternity is not possible or advisable. Donor sperm is used in treatments such as intrauterine insemination (IUI) and in vitro fertilization (IVF), offering a medically supervised, screened, and often legally structured route to conception when partner sperm is unavailable or carries unacceptable health risks. Sperm banks and fertility clinics screen donors for infectious diseases and genetic issues, provide counseling, and maintain records to support informed choices about anonymous or known donation, matching preferences for physical traits or medical history, and managing legal parentage questions. Beyond recipients, donors themselves may gain health screening, counseling, and compensation in some programs, making donation a practical contribution to family-building for many people.

What are the requirements of becoming a sperm donor?
Becoming a sperm donor typically requires that a man be within the donor age range (commonly 18–45 years), be in good general health with no serious chronic conditions, and be willing to provide a full medical, sexual, and family history; clinics also ask about lifestyle, travel, and past infections. Candidates undergo an initial semen analysis to confirm adequate sperm count, motility, and morphology, and comprehensive infectious‑disease screening (HIV, hepatitis, syphilis and other STIs) plus routine blood tests; many programs require genetic carrier screening and sometimes karyotyping to reduce risk of heritable conditions. A physical exam and psychological or counselling assessment are often part of the process to ensure informed consent and to discuss future contact or anonymity rules. Donated samples are usually frozen and quarantined for a period (commonly about six months) while the donor is re‑tested to rule out newly acquired infections before the sperm can be used, and donors must agree to record‑keeping, possible limits on the number of families or births per donor, and legal documentation clarifying parental rights and responsibilities.

How is donated sperm used?
Donor sperm is stored frozen in sperm banks and released to fertility clinics or recipients after required screening and quarantine.
For IUI, thawed donor sperm is washed and placed directly into the uterus around ovulation to increase the chance of fertilization; IUI is commonly used for single women and same‑sex female couples because it is less invasive and less costly.
For IVF, donor sperm is used to fertilize retrieved eggs in the laboratory; when sperm quality or prior fertilization has been problematic, clinics may perform ICSI, injecting a single sperm into an egg to maximize fertilization chances.
Donor sperm is also used to create embryos for gestational carriers or to build embryo banks for future use.
Clinics match donors and recipients based on medical, genetic, and sometimes physical or personal preferences; all donor samples undergo infectious‑disease testing, genetic screening, and record‑keeping to protect recipients and offspring. After fertilization, embryos are transferred to the uterus or frozen for later transfer, and recipients receive medical monitoring and support through pregnancy.

Conclusion
Sperm donation is a safe, regulated pathway that helps build families while balancing medical screening, legal protections, and ethical considerations; donors and recipients should expect thorough testing, counselling, and clear agreements before any use of donated sperm.
Read More
