A vasectomy is a quick, highly effective surgical procedure that provides permanent birth control by blocking the tubes that carry sperm; it does not protect against sexually transmitted infections and requires informed, deliberate consent.
What is a vasectomy?
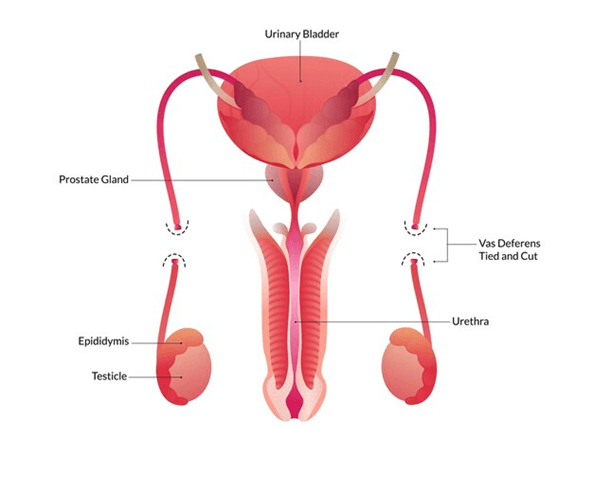
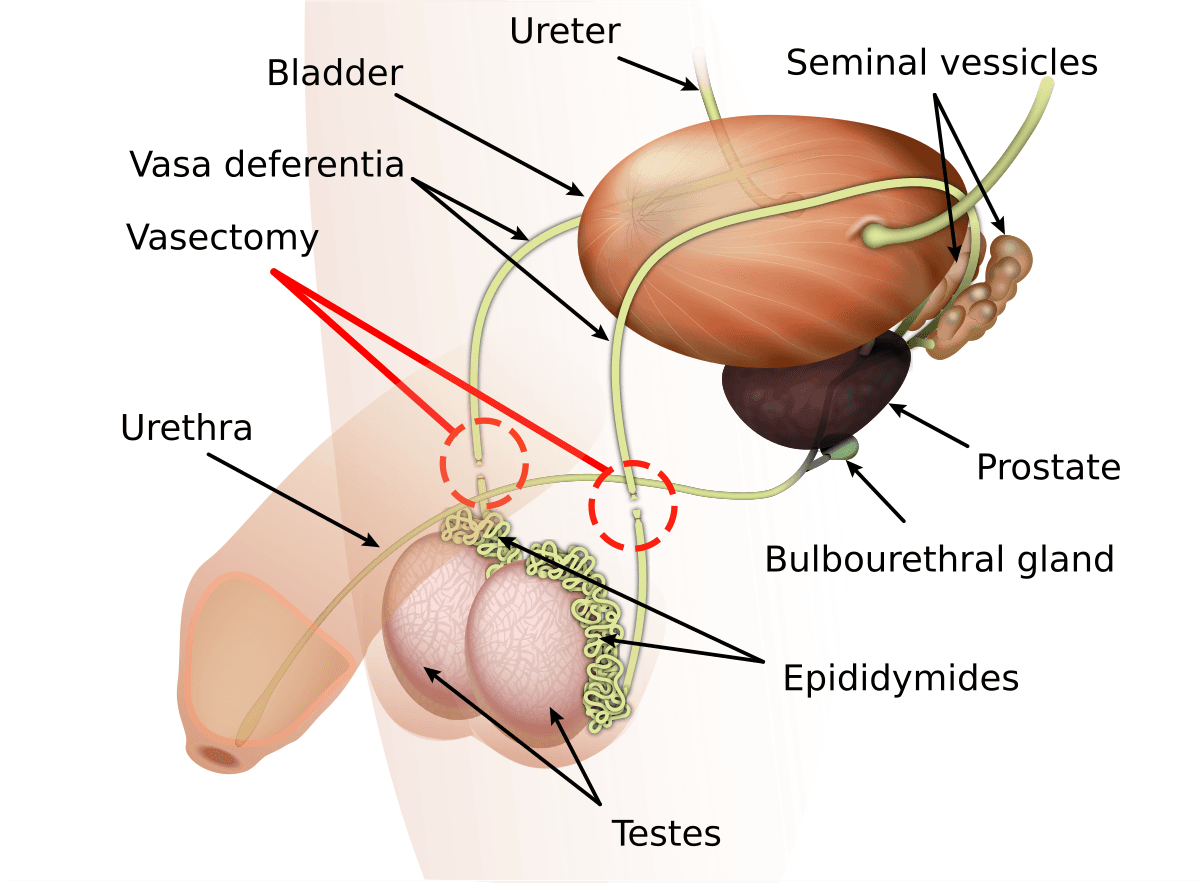
A vasectomy is a minor surgical operation that prevents sperm from mixing with semen by cutting, sealing, or otherwise blocking the vas deferens, the tubes that carry sperm from the testicles to the urethra. The goal is permanent contraception: after the procedure and a confirmed clear semen analysis, pregnancy is extremely unlikely. The procedure is typically brief—often about 20–30 minutes—and is performed as outpatient surgery under local anesthesia, so most people go home the same day and recover quickly. There are two common techniques: the conventional vasectomy, which uses small incisions in the scrotum, and the no‑scalpel vasectomy, which uses a tiny puncture and is associated with less bleeding and faster recovery. During the operation the surgeon locates each vas deferens, then cuts and seals or clips the tube; some clinicians remove a small segment or use cautery to reduce failure risk. You will still ejaculate and have orgasms after a vasectomy, but the semen will not contain sperm once sterility is confirmed. A vasectomy is one of the most effective forms of birth control, but it is not immediately effective—sperm can remain in the reproductive tract for weeks, so use alternative contraception until a follow‑up semen analysis confirms zero sperm. Typical recovery involves mild pain, swelling, and bruising for a few days; most people resume light activity within 48–72 hours and full activity within about a week.

Who gets a vasectomy?
A vasectomy is typically sought by adult men who want a reliable, low‑risk, and permanent form of contraception. Many recipients are men who have completed their desired family size and want to avoid the ongoing costs, side effects, or responsibilities of other contraceptive methods. Couples who jointly decide that no more children are desired often choose vasectomy because it is less invasive, less expensive, and has fewer long‑term health effects than female sterilization. Increasingly, some younger men and those without children are electing vasectomy for personal, financial, or career reasons, or in response to changing social attitudes about shared responsibility for contraception. Men with medical conditions that make pregnancy risky for a partner, or those who face genetic concerns they do not wish to pass on, may also opt for the procedure.
What happens during vasectomy?
A vasectomy typically takes about 20–30 minutes and is performed under local anesthesia as an outpatient procedure; the surgeon locates each vas deferens, then cuts, seals, or blocks the tube—sometimes removing a small segment—to stop sperm from reaching the urethra, and most people go home the same day with minimal downtime. Two common techniques are the conventional vasectomy, which uses small scrotal incisions, and the no‑scalpel vasectomy, which uses a tiny puncture and is associated with less bleeding and faster recovery. During the procedure you remain awake but numb, and normal ejaculation and sexual function continue because the testes still produce hormones and fluid; only sperm are prevented from entering the semen. Because sperm can remain in the reproductive tract after surgery, alternative contraception must continue until a follow‑up semen analysis confirms zero sperm, which usually occurs after several weeks or a specified number of ejaculations.
What are the risks & benefits of a vasectomy?
A vasectomy’s primary benefit is durable, near‑complete prevention of pregnancy: once follow‑up semen analysis confirms absence of sperm, the procedure is more than 99% effective and eliminates the need for ongoing contraception for couples who are certain they want no future biological children. The operation is typically quick, performed under local anesthesia in an outpatient setting, and recovery is short—most men resume light activity within a few days—so it is often favored over female sterilization for its simplicity, lower cost, and fewer perioperative risks. Additional benefits include avoidance of daily or partner‑dependent methods, reduced long‑term contraceptive expense, and preservation of sexual function because hormone production and ejaculation remain intact.
Risks and trade‑offs include immediate surgical risks—bleeding, infection, and hematoma—and a small but real chance of failure that can lead to pregnancy if sperm persist or the vas deferens spontaneously reconnects; follow‑up semen testing is essential to confirm sterility. A minority of men experience chronic scrotal or testicular pain (post‑vasectomy pain syndrome), which can be persistent and sometimes difficult to treat. Psychological regret is another consideration: because vasectomy is intended as permanent contraception, men who later desire biological children may need reversal surgery or assisted reproduction, both of which are costly and not guaranteed to succeed.
Vasectomy recovery time
A typical vasectomy recovery begins immediately after the procedure with mild soreness and pressure in the scrotum; applying ice, wearing supportive underwear, and resting for the first 24–48 hours helps control discomfort and swelling. Many men feel well enough to resume light, nonstrenuous activity within 48–72 hours, though individual pain tolerance and the exact technique used (no‑scalpel vs conventional) affect the timeline. Bruising and localized swelling are common and usually peak in the first few days before steadily improving; most people report that routine daily tasks are manageable within a few days, while full comfort and normal exercise or heavy lifting are typically resumed after about one to two weeks.
Recovery continues beyond symptom relief because sperm can remain in the reproductive tract for weeks; alternative contraception must be used until a follow‑up semen analysis confirms zero sperm, which commonly occurs after several weeks or a specified number of ejaculations. A day‑by‑day approach helps: take the day of the procedure off, rest the next 24–48 hours, gradually increase activity over the first week, and avoid vigorous exercise or heavy lifting for about seven days to reduce bleeding risk. If swelling, increasing pain, fever, or a growing lump occur, contact your provider promptly as these can indicate infection or hematoma that may need treatment.
Conclusion
A vasectomy is a safe, highly effective form of permanent contraception that offers quick recovery and long‑term pregnancy prevention, but it requires informed consent, follow‑up semen testing, and consideration of irreversible trade‑offs.
Read More
