An orchiectomy is a surgical procedure that removes one or both testicles; its most commonly performed to treat suspected or confirmed testicular cancer, to lower testosterone for prostate cancer, or as part of gender-affirming care.
What is orchiectomy?
An orchiectomy (also spelled orchidectomy) is a surgical operation to remove one or both testicles, the male reproductive organs that produce sperm and the hormone testosterone. The procedure may be unilateral (removing one testicle) or bilateral (removing both) and is performed for several medical reasons: to diagnose or treat testicular cancer, to reduce testosterone in advanced prostate cancer, to remove irreparably damaged testes after trauma or infection, or as part of gender-affirming surgery for some transgender and non-binary people. The most common cancer-related approach is a radical inguinal orchiectomy, in which the testicle is removed through a groin incision to avoid spreading tumor cells; a simple orchiectomy through the scrotum may be used for palliative or non-cancer indications. Recovery is generally straightforward with short-term pain, swelling, and activity restrictions; many patients go home the same day. When both testicles are removed, testosterone levels fall, which can cause decreased libido, fatigue, and bone density loss, and may prompt discussion of hormone replacement. Fertility is affected if both testes are removed, so sperm banking is often discussed beforehand when future fertility is a concern.

Why do people get an orchiectomy?
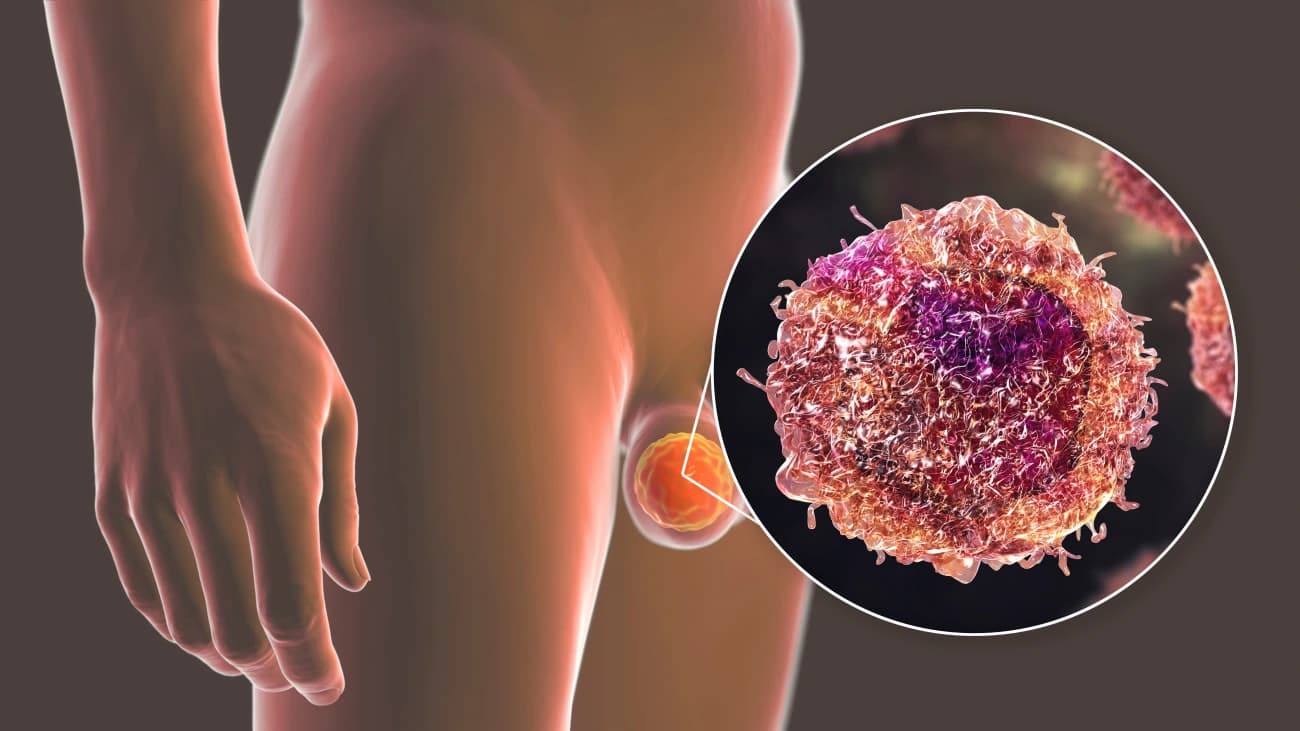
An orchiectomy is most commonly done when there is a strong suspicion or confirmation of testicular cancer, because removing the affected testicle both establishes a definitive diagnosis and removes the primary tumor; for suspected cancer the standard approach is a radical inguinal orchiectomy, which minimizes the risk of spreading tumor cells during surgery. People also undergo orchiectomy when a testicle is severely damaged by trauma, infection, or torsion and cannot be repaired; in these cases removal prevents ongoing pain, infection, or other complications and may be the safest option to preserve overall health. For advanced prostate cancer, bilateral orchiectomy can be used to rapidly lower testosterone levels and slow hormone‑sensitive tumor growth, offering a surgical alternative to medical hormone suppression. When both testicles are removed, fertility is lost and testosterone production falls, so clinicians commonly discuss sperm banking and hormone replacement before surgery if preserving fertility or maintaining hormonal balance is desired.
How to prepare for an orchiectomy?
Before an orchiectomy, confirm the exact procedure planned with your surgeon—whether it will be a radical inguinal approach for suspected cancer or a simple scrotal approach for noncancer reasons—and review the risks, benefits, and alternatives so you know what to expect. Complete any required preoperative tests such as blood work, imaging, or ECG as directed; these help assess fitness for anesthesia and identify issues that could change the surgical plan. If there is any chance you want children in the future and bilateral removal is possible, discuss sperm banking with your care team well before surgery because orchiectomy can cause permanent infertility. For patients who may need ongoing testosterone, ask about hormone replacement options and how removal will affect symptoms like libido, energy, and bone health.
What happens during an orchiectomy?
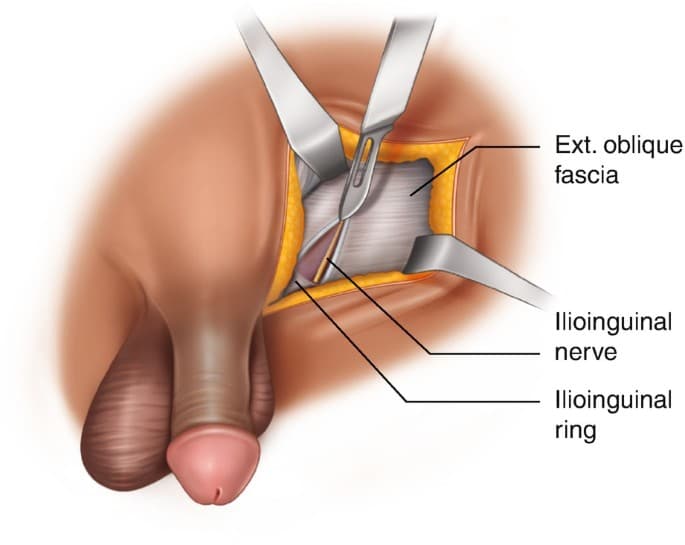
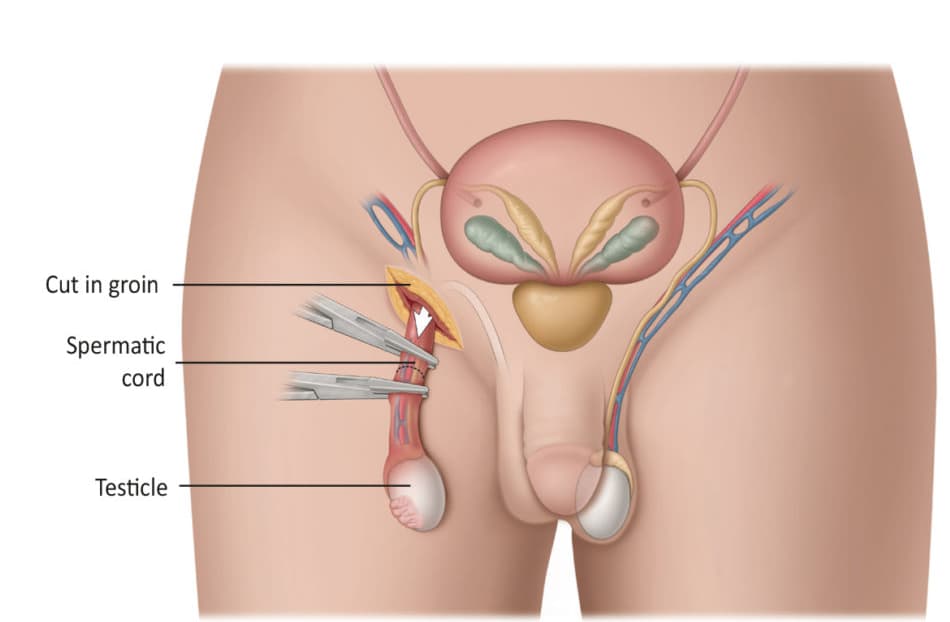
During an orchiectomy the patient receives anesthesia and the surgical team prepares the groin and scrotal area with antiseptic; for suspected cancer the standard is a radical inguinal approach where a small incision is made in the groin to access the spermatic cord and testicle, minimizing the chance of spreading tumor cells. The surgeon isolates and ligates the spermatic cord, then removes the testicle and cord as a single specimen for pathological examination. If the indication is noncancerous—such as severe trauma, infection, or palliative hormone control—a simple scrotal approach may be chosen and the testicle removed through the scrotum. Hemostasis is achieved, the wound is irrigated, and the incision is closed with absorbable or nonabsorbable sutures; a scrotal support or dressing is applied to reduce swelling. The operation typically lasts under an hour, and most patients recover in a postanesthesia area before discharge the same day. Short‑term effects include pain, swelling, and bruising; bilateral orchiectomy causes a permanent drop in testosterone and infertility, so preoperative counseling about sperm banking and hormone replacement is important. Follow‑up includes wound checks, activity restrictions, and further cancer staging or treatment if needed.
What are the risks & benefits of orchiectomy?
An orchiectomy can be curative or palliative depending on the indication: removing a testicle with a tumor both establishes a definitive diagnosis and eliminates the primary cancer source, and bilateral orchiectomy rapidly lowers testosterone to slow hormone‑sensitive prostate cancer, often more quickly and reliably than medical therapy. For people with irreparably damaged testes from trauma, torsion, or infection, orchiectomy relieves pain and prevents ongoing complications. When performed as part of gender‑affirming care, orchiectomy can align physical characteristics with gender identity and reduce the need for long‑term antiandrogen medications.
However, the procedure is not without downsides: short‑term surgical risks include bleeding, infection, hematoma, and wound complications, while long‑term consequences after bilateral removal include permanent loss of fertility and sustained low testosterone with effects on libido, energy, mood, and bone density; these outcomes often require counseling about sperm banking and consideration of hormone replacement therapy. There is also a small risk of chronic scrotal or groin pain and, rarely, hernia or nerve injury. For cancer patients, orchiectomy may be the first step in a broader treatment plan that could include imaging, chemotherapy, or lymph node surgery.

Orchiectomy recovery process
An orchiectomy recovery typically begins in the post‑anesthesia care unit where nurses monitor vital signs and pain; most patients are discharged the same day once stable and able to urinate and tolerate oral fluids, with instructions for wound care, activity limits, and pain medication. Short‑term symptoms commonly include localized pain, swelling, bruising, and scrotal tightness; using ice packs, wearing supportive underwear or a scrotal support, and taking prescribed analgesics helps control discomfort and reduce swelling. Patients are usually advised to avoid heavy lifting and strenuous exercise for about six weeks, but many can return to desk work or light daily activities within two to three weeks depending on pain and the surgeon’s guidance. Wound care involves keeping the incision clean and dry, watching for increasing redness, drainage, or fever, and following instructions about when to remove dressings or sutures; contact the surgical team promptly for signs of infection or hematoma. If the orchiectomy was cancer‑related, recovery also includes staging discussions and possible further treatment such as imaging, chemotherapy, or lymph node evaluation, so early follow‑up appointments are scheduled to review pathology and plan next steps. Important considerations before and after surgery include fertility and hormonal effects: bilateral orchiectomy causes permanent infertility and a sustained drop in testosterone, so clinicians commonly discuss sperm banking before surgery and testosterone replacement options afterward when appropriate. For patients concerned about body image, a testicular prosthesis can be placed later or at the time of surgery depending on preference and clinical factors. Most people see steady improvement over weeks to months; persistent or worsening pain, fever, increasing swelling, or wound drainage warrant urgent evaluation.
Conclusion
Orchiectomy is a well‑established surgical option that can be curative for testicular cancer, provide rapid androgen suppression for hormone‑sensitive disease, or relieve symptoms from irreparably damaged testes; it carries predictable surgical risks and important long‑term consequences that require preoperative planning and postoperative support.
Read More
