The pancreas is a dual‑function gland that plays a central role in digestion by producing and delivering digestive enzymes into the small intestine while also secreting hormones into the bloodstream that regulate metabolism.
What is a pancreas?
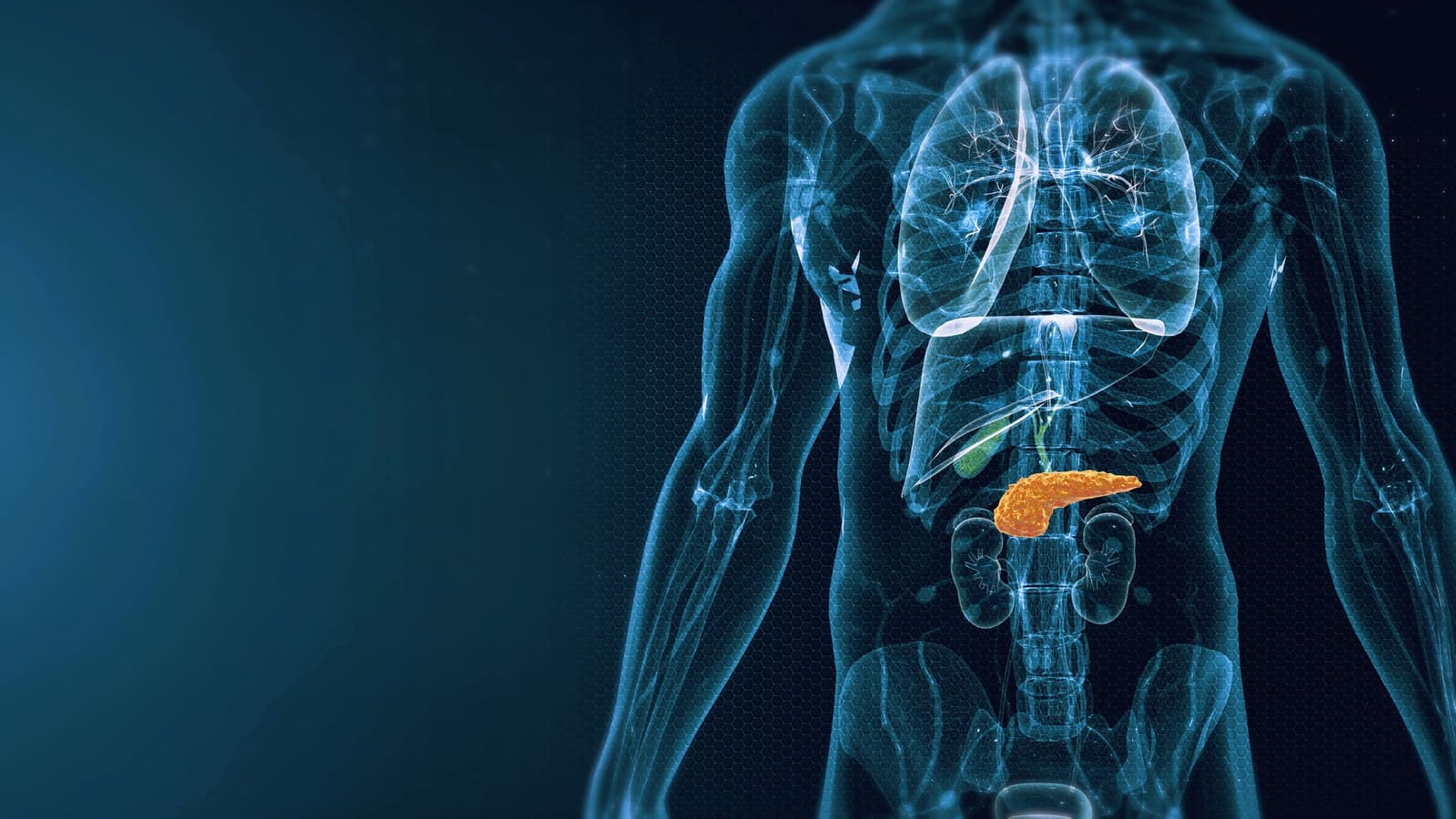
The pancreas is a soft, elongated gland tucked deep in the upper abdomen behind the stomach that performs two essential roles for digestion and metabolic balance: an exocrine function that produces digestive enzymes (amylase, lipase, proteases) delivered into the duodenum to break down carbohydrates, fats, and proteins, and an endocrine function in which clusters of islet cells secrete hormones (insulin and glucagon) into the bloodstream to regulate blood glucose; this dual, or heterocrine, nature makes the pancreas indispensable for nutrient absorption and energy homeostasis. Anatomically it lies transversely across the posterior abdominal wall, with a head near the duodenum, a body crossing the midline, and a tail approaching the spleen, and it drains via a ductal system into the biliary tree. Healthy pancreatic secretions are alkaline and neutralize stomach acid while providing concentrated enzymes that act in concert with bile to emulsify and digest food. Damage to the gland—by gallstones, alcohol, metabolic disorders, genetics, autoimmune disease, or tumors—can produce inflammation, malabsorption, pain, or diabetes, and because of its deep location symptoms are sometimes subtle, requiring laboratory tests and imaging for diagnosis.
What does the pancreas do?
The pancreas is a multipurpose gland that performs two essential roles for digestion and metabolic balance: exocrine and endocrine functions. Its exocrine cells produce pancreatic enzymes—amylase to break down carbohydrates, lipase to digest fats, and proteases to cleave proteins—which are delivered through ducts into the duodenum where they neutralize acidic stomach contents and complete the chemical digestion necessary for nutrient absorption. Simultaneously, the endocrine islets secrete hormones into the bloodstream—primarily insulin and glucagon—that regulate blood glucose by promoting cellular uptake of glucose after meals or releasing stored glucose during fasting, thereby maintaining energy homeostasis. These coordinated activities link food breakdown with systemic metabolic responses: efficient enzyme secretion enables caloric and fat‑soluble vitamin absorption, while proper hormonal signaling prevents hyperglycemia or hypoglycemia. When exocrine output falls, patients develop malabsorption, oily stools, and weight loss; when endocrine function is impaired, diabetes can result. The pancreas also contributes to appetite and digestive timing through hormonal signals that influence stomach emptying and satiety. Because it integrates digestive chemistry with hormonal control of metabolism, preserving pancreatic health is vital for nutrition, energy regulation, and overall well‑being.
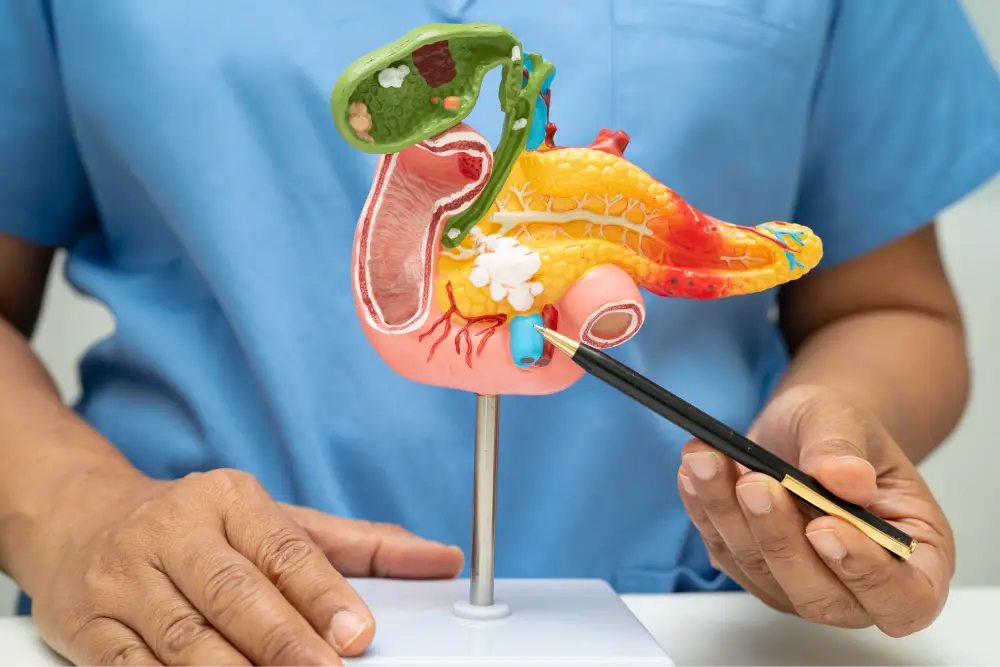
What is the role of your pancreas in digestion?
The pancreas plays a central role in digestion by combining powerful exocrine and endocrine functions that together enable nutrient breakdown, absorption, and metabolic regulation: its exocrine acinar cells produce pancreatic enzymes—amylase for carbohydrates, lipase for fats, and proteases such as trypsin and chymotrypsin for proteins—that are secreted as an alkaline juice into the duodenum to neutralize stomach acid and chemically break food into absorbable molecules, working together with bile to allow efficient uptake of fats and fat‑soluble vitamins; concurrently, the pancreas’ endocrine islets release hormones into the bloodstream—primarily insulin and glucagon—that coordinate postprandial glucose uptake, hepatic glucose production, and overall energy balance, while other peptide hormones modulate appetite, gastric emptying, and digestive secretions; when exocrine output is deficient, patients develop malabsorption, oily stools, and weight loss, and when endocrine output fails, glucose regulation is impaired and diabetes can result, illustrating how loss of either function disrupts nutrition and systemic metabolism and why preserving pancreatic health and timely treatment of disease are essential for digestion and whole‑body homeostasis.
Common pancreatic problems and digestion
Common pancreatic problems — diabetes, pancreatitis, and pancreatic cancer — each disrupt digestion and metabolism in distinct but overlapping ways, often producing malabsorption, weight loss, and systemic illness.
Diabetes arises when the pancreas’ endocrine islets fail to secrete adequate insulin or when insulin action is impaired, leading to altered glucose handling that affects appetite, nutrient utilization, and long‑term metabolic health.
Pancreatitis, an acute or chronic inflammatory condition, injures exocrine acinar cells and ductal tissue, reducing secretion of pancreatic enzymes (lipase, amylase, proteases) needed to break down fats, carbohydrates, and proteins; enzyme loss produces oily, foul‑smelling stools, nutrient deficiencies, and weight loss, while acute severe attacks can cause systemic inflammatory response and organ dysfunction.
Pancreatic cancer can obstruct the pancreatic or bile ducts and destroy both exocrine and endocrine tissue, causing progressive malabsorption, jaundice, painless weight loss, and sometimes new‑onset diabetes; ductal blockage further impairs enzyme delivery to the intestine and worsens digestive failure.
Because these conditions compromise enzyme production, hormonal balance, or anatomic flow, their management routinely includes nutritional support, pancreatic enzyme replacement when indicated, glucose control for endocrine failure, and targeted therapies (endoscopic, surgical, oncologic) to restore digestion and quality of life.

Conclusion
The pancreas is indispensable to efficient digestion and metabolic balance because it delivers both the chemical tools and hormonal signals the body needs to process food and regulate energy: its exocrine enzymes (amylase, lipase, proteases) neutralize stomach acid and break carbohydrates, fats, and proteins into absorbable components in the duodenum, while its endocrine hormones (insulin, glucagon, and other peptides) coordinate how absorbed nutrients are stored, released, and used by tissues. Because many pancreatic diseases — from acute and chronic pancreatitis to tumors and metabolic disorders — simultaneously affect enzymes and hormones, their impact extends beyond local symptoms to systemic nutrition and metabolic health.
Read More
